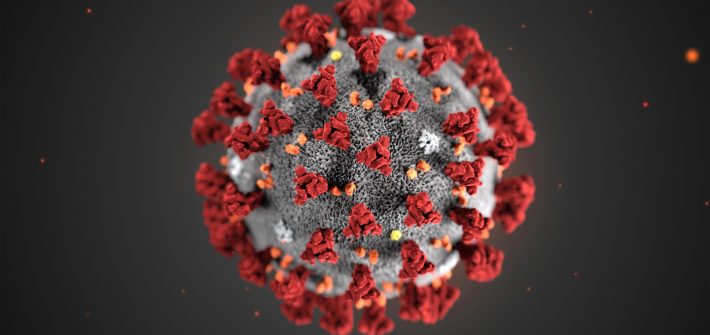
How to cope with the stress of coronavirus / Covid-19 and self-isolation
Tips
Mindfulness: The top 5 best mindfulness apps

Mindfulness has been trendy for a while, but it’s a bit more than just a fad! The NHS have approved its use with a variety of mental health difficulties. Most often prescribed for use with recurrent depression, frequently cited as helpful with anxiety, some studies show it helps with managing chronic pain; so if these […]
Cognitive Behavioural Therapy – Tips For Therapists

Here are some tips taken from the CBT bible, Back to Basics, by Beck to help therapists carry out their work in the most effective way. Clients can be fearful of what to expect from treatment so it will help to set an agenda at the start of each session. This also allows you to […]
CBT – Core Beliefs

Core beliefs in CBT We all have central beliefs are about ourselves and our relations to others; they are like short cuts to which we revert, time after time. The problem arises when they become maladaptive, and in which case they often highlight an underlying belief about us being one of three things: unlovable, helpless […]
CBT – Intermediate Beliefs
Intermediate Beliefs are different from core beliefs and encorporate rules, attitudes and assumptions. We formulate these gradually through treatment, not right from the start. It can help to explain that different people have different beliefs because of different personalities and experiences, and that they may make things hard for us but that we can unlearn […]
Acceptance and Commitment Therapy – Separating Thoughts from Feelings
Our thoughts and feelings can become fused, and when they are, they become distressing to us, but we don’t have to let them rule our actions and the meaning we get from life. Fusion happens when we create the following within our minds: Rules Reasons and justifications Judgements Thoughts about the Past Thoughts about the […]
Acceptance and Commitment Therapy – Committed Action

When we are faced with challenging situations, distressing feelings, emotions and even pain and fatigue it is important to continue living a life which is as close to our values as possible. This can allow us to gain meaning, achievement and enjoyment from life despite these obstacles. Values Values can be imagined as a direction, […]
- Depression
- ...
Bereavement, Grief, Mourning and Loss

So I went on a training day about bereavement and loss, because many of the people I treat have experienced one of these, and for some of them it is this loss which stops them from moving forward. I felt I needed the training because I haven’t gone through that much loss myself and I […]
The best Cognitive Behavioural Therapy apps / CBT apps

There’s lots of evidence that Cognitive Behavioural Therapy (CBT) is effective at treating anxiety, depression, phobias, hypochondria, PTSD and eating disorders. Trouble is…whilst it’s free on the NHS, the waiting lists are huge; where I work, clients have to wait up to 6 months for treatment in some cases! Of course you can pay, but […]
How to Relax – Progressive Muscular Relaxation

People with anxiety difficulties are often so tense throughout the day that they don’t even recognize what being relaxed feels like. Progressive Muscle Relaxation is a scientifically proven way to help you relax and to teach your body how to recognise the signs of stress, tension and anxiety. Do it regularly (try once a […]