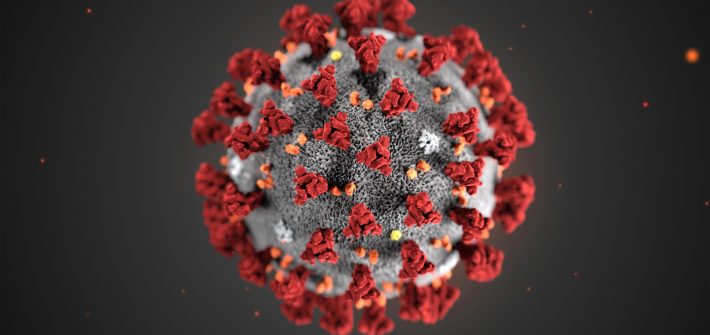
How to cope with the stress of coronavirus / Covid-19 and self-isolation
Panic
- Anxiety
- ...
Panic Disorder Management – a problem based learning case study

Often, when we are presented with a case it can be difficult to find a way forward. To aid clinical decisions, it is sometimes necessary to break down the decision making process into stages. The problem based learning task below does just that. Here I was given a case study and we methodically worked through […]